About the research
Our research examines the impact of existing welfare systems and the prospective impacts of Basic Income on public health, service provision and a range of other social and economic outcomes. Basic Income is a system of regular, secure, predictable payments to all individuals. Unlike most existing welfare systems, it is not ‘means-tested’ (dependent on low income), based on additional needs (such as those related to being disabled), or dependent on particular behaviour (such as being unemployed and looking for work). While there may be a small number of situations where payments could be withdrawn, for example due to serious criminal behaviour, for the overwhelming majority it would be unconditional and paid forever. We develop evidence-based policy proposals around Basic Income that address key modern challenges and achieve public support. We use collaboration with organisational partners, such as Compass, Autonomy and the RSA, to translate research into real-world impact.
Key messages
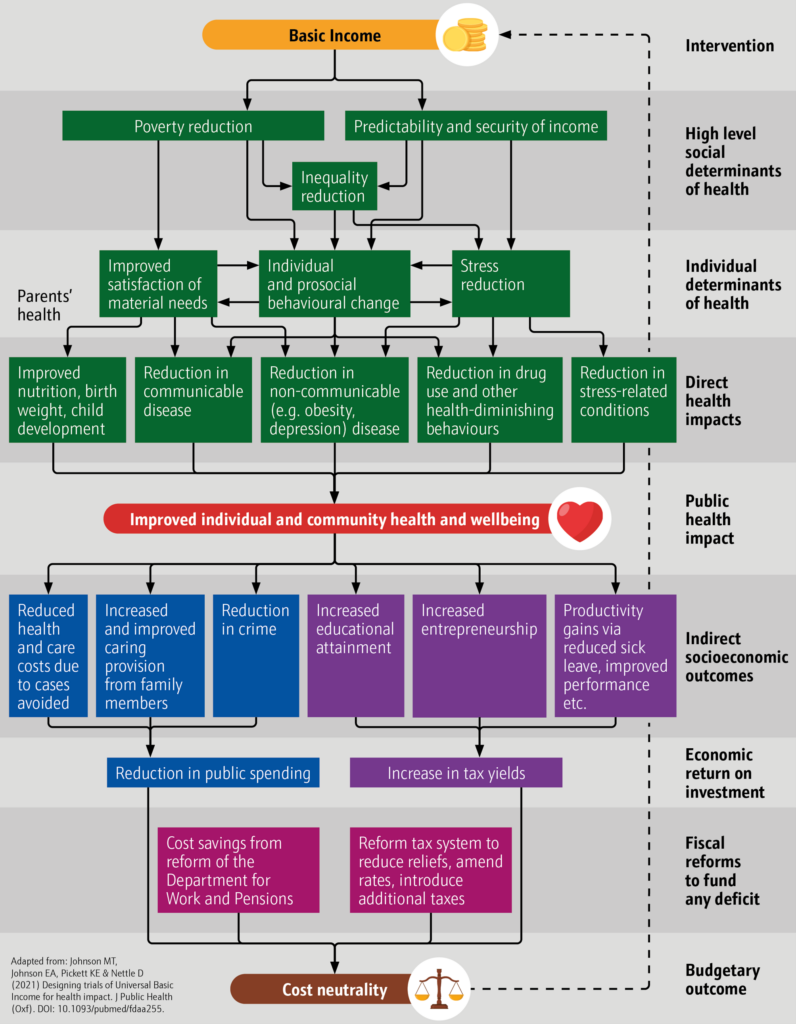
Our model of impact suggests that Basic Income can promote public health by:
- Addressing poverty, which increases people’s ability to satisfy their basic needs, for example helping them to afford better food and housing.
- Reducing inequality, giving people the option to leave abusive, damaging environments, which reduces stress and stress-related illnesses.
- Providing a predictable and secure income, lengthening people’s perceived lifespan and promoting healthy behaviours.
For a larger version of this image please click here.
The challenge
A large body of evidence indicates the importance of understanding social determinants of health (e.g. The Marmot Review, Lancet Public Health and Equality and Human Rights Commission). While awareness of social determinants has increased steadily since publication of the Black Report in 1980, there is genuine disagreement about the nature and identity of those determinants and the relationship between income and health in particular. Positions are often shaped by disciplinary background, but explanations range from there being little meaningful impact of income on health, at least directly, to the relationship being causally bi-directional with roughly equal effects in both directions, to income’s having a highly determinate impact on health (e.g. Thompson et al., Cooper & Stewart and Benzeval et al.). Reasons for disagreement include the lack of natural experimental or randomised controlled trials of sufficient size and scale, but these are often restricted to discussion of domestic policy, since development and aid policy assume that income has a high degree of determinacy on health.
In the absence of Basic Income trials of sufficient size, duration and generosity, there is urgent need to provide policymakers with evidence by which to assess the case for developing and implementing pilots, trials and schemes. Given concern about the impact of qualitative methods in shaping public health policy, this requires complex analysis of existing large longitudinal datasets.
This work includes analysis of relationships between income, financial security and a range of health measures, as well as microsimulation of distributional and health impacts on the basis of trends identified within the datasets.
The approach
Our research programme is fundamentally interdisciplinary, involving a range of quantitative and qualitative methods, with commitment to ensuring that approaches complement and support claims made. Our engagement with UK Data Service resources has focused on analysis of the relationship between income, financial security and health. This work has provided estimates of the probabilities of mental and physical ill-health based on socioeconomic status (SES) and microsimulation of distributive and health impacts from introduction of Basic Income schemes.
In Parra-Mujica et al. (2023), we examined the relationship between socioeconomic status and mental health among 16- to 24-year-olds using 10 waves of Understanding Society: The UK Household Longitudinal Study (UKLHS). We examined the relationship between measures of mental health using the Mental Component Summary (MCS) of the Short-Form Health Survey (SF-12), which has been used to screen for general, non-psychotic mental health problems among primary care patients, and measures of socioeconomic status, using net equivalised household income, which is the sum of net monthly incomes from all household members, adjusted by the OECD-modified equivalence scale to account for households of different size and composition.
In Villadsen et al. (2023), we examined the relationship between socioeconomic status and mental health among 14- and 17-year-olds in the Millennium Cohort Study (MCS) and 25-year-olds in Next Steps (NS). The MCS is highly multi-disciplinary with a rich and diverse set of variables, including income and socioeconomic circumstances of parents and assessments of mental health of both cohort members and parents. The cohort member measures of mental health were the Short Moods and Feelings Questionnaire (SMFQ) at age 14, Kessler 6 (K6) at age 17, and the General Health Questionnaire (GHQ-12) at 25. We also controlled for the mental health of main parents or guardians in some of our MCS analyses using K6 when the cohort member was 17 and the Malaise Inventory when the cohort member was aged 9 months. We used net equivalized household income, parent or guardian financial strain, cohort member assessed relative family wealth, highest in household occupational classification (NS-SEC), highest in household education and socioeconomic deprivation indices to measure socioeconomic status.
In Reed et al. (2023), we used the Family Resources Survey (FRS) from the 2019/20 fiscal year to microsimulate the tax-transfer distributional effects of Basic Income cash payments of different levels and then, in Chen et al. (2023), combined this analysis with UKHLS estimates from Parra Mujica et al. (2023) to microsimulate the impact of the distributional changes on anxiety and depression among 14-to 24-year-olds. For the years before 2019/10 that we modelled, we deflated the Basic Income payments using the UK Consumer Prices Index, with the income tax and National Insurance increases adjusted in each wave to ensure approximate fiscal balance and to compensate for any change in real incomes between UKHLS waves.
As a result of our work in this area, members of the team (Elliott Johnson and Howard Reed) were invited to take part in the Understanding Society Health Challenge: Research Springboard, a three-day workshop series which took place between March and May 2023. This resulted in a collaborative project with academics from UCL and the University of Bristol, with a journal article planned, and a Working Paper (Coates, Patel & Vanner 2023).
Data used from the UK Data Service collection
The UK Data Service’s collection of longitudinal panel data provides unparalleled access to data on the relationship between income, financial security and a range of health conditions over time. Not only does it permit comparison between datasets, it also enables contextualisation of qualitative work in specific communities as well as smaller studies of natural experiments, such as The Changing Cost of Living study. In this vein, the availability of large longitudinal panel datasets has also been instrumental in shaping generic, adaptive protocol resources for the study of Basic Income Pilots and Trials (Johnson et al. 2023).
Key data from the UK Data Service included the following datasets:
- Family Resources Survey
- Millennium Cohort Study
- Next Steps (previously the Longitudinal Study of Young People in England (LSYPE1))
- Understanding Society
Research findings
Income, financial security and perception of inequality are key drivers of health outcomes (Villadsen et al. 2023; Parra-Mujica 2023)
The researchers found that being in a higher income group is associated with a reduced likelihood of clinically significant depressive symptoms, whilst those living in the poorest households have a greater probability of mental health problems than the richest. Alongside this, increases in income over the course of childhood and adolescence are associated with reduced symptoms of depression and anxiety.
Basic Income as a means of improving income and financial security is impactful as a preventive and responsive public health strategy (Chen et al. 2023; Johnson, Reed et al. 2023)
Increases in income and higher average income is associated with better mental and physical health, there is also a relationship between lower income and worse mental and physical health. Basic income would likely have a very significant impact as a preventive health measure. For example, based on depressive disorders, NHS and personal social service cost savings could be between £125 million and £1.03 billion assuming 50% of cases diagnosed and treated.
Basic Income is affordable (Reed et al. 2023)
An argument against Basic Income is that it is not affordable. The researchers used microsimulation of data from the Family Resources Survey to outline the impacts and costs of three different Basic Income Schemes. Even the fiscally neutral starter scheme proposed would lead to poverty rates in children and pensioners below their post-1961 low points. The more generous schemes would make further inroads into reducing the UK’s levels of poverty and inequality, but at greater cost. All of this could be done in the timeframe of one parliament.
Basic Income is popular (Johnson, Johnson, Reed & Nettle 2023)
The research showed that policies such as Basic Income can attract votes and deliver greater control, certainty and predictability for politicians and political parties. When properly framed, redistributive policies have the capacity to persuade votes. People prefer systems that reduce poverty and ideally would like a system that removes it altogether.
Trials can be evaluated much more effectively to understand health impact (Johnson, Johnson, et al. 2023)
Evaluations of upstream cash transfer trials have historically failed to capture impacts on health. This research has described a process by which this can be improved not only in the UK but also in low- and middle-income countries. It can be used for not only Basic Income trials but other welfare system changes.
Recommendations for policy
We have set out a series of recommendations for policymakers across several reports for Compass, Autonomy and RSA. These are that:
- Policymakers should commit to trials of Basic Income.
- Policymakers with an interest in public health should explain the material health and economic benefits of Basic Income to voters using narratives tailored specifically to people’s circumstances.
- Trials should be evaluated comprehensively and consistently using measures that enable comparison with longitudinal datasets administered by the UK Data Service.
- More microsimulation modelling should be undertaken to cover all age groups and all major health conditions.
- Researchers and policymakers must engage in co-production with stakeholders to determine formulation of schemes and means of funding.
- Copyrighted evaluation measures should be brought into the public domain
The impact
This programme of research used a wide-ranging body of evidence on the health, social and economic impacts of Basic Income to persuade policymakers, third sector organisations and community groups to support the policy. Impact is evident in several areas:
Persuading policymakers of the health, social and economic benefits and to commit publicly to Basic Income.
The research and reports received with contributions and endorsements by Mark Drakeford, First Minister of Wales, Jamie Driscoll, Mayor of North of Tyne, Andy Burnham, Mayor of Greater Manchester, Ian Lavery MP (see Johnson, Webster et al. 2022; Johnson, Nettle et al. 2022).
“This report sets out how Universal Basic Income, a radical yet feasible alternative to the existing, failing benefits system, could begin to address these issues [of financial and mental wellbeing for young people]. Universal Basic Income would reduce poverty to almost unheard-of levels, address the inequality both between and within regions that harms people’s wellbeing, and provide a foundation for our young people to secure good lives that support good mental health. Most importantly, the report confirms that our people see this as an important policy – something that can transform their lives at a time in which they need change most.”
Mayor of Greater Manchester, Andy Burnham
“Over the course of this trial [of a Basic Income for care leavers], we will be able to test the many claims made about Basic Income, but we hope it will support a national consensus that Basic Income has a central role to play in addressing inequality and in ensuring our young people have the same opportunities to fulfil their potential as each other.”
Rt Hon Mark Drakeford MS, First Minister of Wales
“This Compass report shows us that the idea of a universal basic income is more popular than you might think. And for good reasons: it offers the single biggest improvement in working people’s interests for a generation. It increases economic security for the young and reduces the risks of ill health for the old. It’s also simpler to run and easier to navigate than the existing social security system. Complexity is our enemy when it comes to tackling poverty and inequality.”
North of Tyne Mayor, Jamie Driscoll
Raising the media profile of Basic Income
Design of payment levels within community-led micropilots in England with community groups and third sector organisations, which has received widespread media coverage including coverage on the BBC2 Politics Live, James O’Brien on LBC, Sky, ITV Tyne Tees News, and in the Guardian, BBC, Daily Mail, Independent, The Sun, Daily Mirror, Evening Standard, Daily Express, LBC, Linked In, among others. The coverage has fostered debate on the broader issues and policy, with the Independent committing its support to Universal Basic Income.
The micropilot was also discussed in the House of Commons (Cowan 2023) and Sadiq Khan, Mayor of London, highlighted the micropilot in the London Assembly (Polanski 2023) and stated his plan to follow the scheme and the results of it.
Influencing evaluation methods of cash transfers
This research presented the first generic, adaptive protocol for evaluation of cash transfers capable of presenting evidence (Johnson, Goodman et al. 2023). This has informed development of the evaluation protocol for the Welsh Basic Income Pilot for Care Leavers and community-led micropilots.
Putting the spotlight on basic income amongst other researchers
The researchers worked through Understanding Society Health Challenge: Research Springboard to understand the relationship between different measures of income and health and to emphasise the need for consistency of measures in studies of upstream interventions (Coates, Patel & Vanner 2023). The opportunity to engage with Understanding Society, and other researchers, allowed the researchers to highlight the importance of UBI and the role it can play.
Helping people “on the ground”
Beneficiaries of the impact include party policymakers, community organizations, NGOs and charities, health professionals and the general public. For example, Dr Jonathan Coates, GP in Newcastle upon Tyne and NIHR In-Practice Fellow, Durham University gave the following feedback on the Basic Income micropilot (see Johnson, Goodman et al. 2023):
“Put simply, financial precarity is making people sick, something I see increasingly in my clinical work. The detailed modelling in this report suggests that Basic Income could significantly reduce this precarity, with consequent positive effects on health and wellbeing. The opportunity to make a concrete difference to health outcomes is exciting both at the level of individual patients and communities, but also from the perspective of the NHS as we wrestle with increasing demand. The report shows that the public understand this and, crucially, are supportive of bold measures to try and improve things. Basic Income represents an opportunity to follow in the footsteps of previous bold interventions to address the causes, not the symptoms, of illness.”
Dr Jonathan Coates
Residents and participants taking part in the pilot scheme voiced their support for the scheme and also pointed out some potential benefits:
“There are people who can’t see beyond a week or month. Holidays, culture and activities are blocked off to them. In areas of the North-East, we suffered through industrial changes in the 1980s. The inequalities between here and the rest of the country are huge. UBI could improve the health profile of the region”
“[Basic income] gives the ability to do something different, for example travel, different jobs, support for artists”
“[Basic income] helps give people dignity. If disabled [you would] not have to jump through hoops. The dignity aspect is really bad at the moment”
Read the research
Articles
Chen, T., Reed, H., Parra-Mujica, F., Johnson, E. A., Johnson, M., Collins, B. & Kypridemos, C. (2023) ‘Quantifying the mental health and economic impacts of prospective Universal Basic Income schemes among young people in the UK’, BMJ Open. DOI: 10.1136/bmjopen-2023-075831.
Johnson, E. A., Reed, H. & Johnson, M. T. (2023) ‘Can Universal Basic Income work for disabled people? An examination of existing UK organisational and academic positions’, Disability & Society. DOI: 10.1080/09687599.2023.2233688.
Johnson, E. A., Johnson, M. T., Kypridemos, C., Villadsen, A. & Pickett, K. (2023) ‘Designing a generic, adaptive protocol resource for the measurement of health impact in cash transfer pilot and feasibility studies and trials in high-income countries’, Pilot and Feasibility Studies. DOI: 10.1186/s40814-023-01276-4.
Johnson, M. T., Johnson, E. A., Reed, H. & Nettle, D. (2022) ‘Can the downward spiral be stopped? Balancing transformative policy with feasibility in red wall constituencies’, British Journal of Politics & International Relations. DOI: 10.1177/13691481221146886.
Parra-Mujica, F., Johnson, E. A., Cookson, R. & Johnson, M. T. (2022) ‘Understanding the relationship between income and mental health among 16- to 24-year-olds: Analysis of 10 waves (2009-2020) of Understanding Society to enable modelling of income interventions’, PLOS One. DOI: 10.1371/journal.pone.0279845.
Reed, H., Johnson, M. T., Lansley, S., Johnson, E. A., Stark, G. & Pickett, K. (2023) ‘Universal Basic Income is affordable and feasible: evidence from economic microsimulation modelling’, Journal of Poverty and Social Justice, 31:1, 146-162. DOI: 10.1332/175982721X16702368352393.
Villadsen, A., Johnson, E. A., Cookson, R. & Johnson, M. T. (2023) ‘How far can interventions to increase income improve adolescent mental health? Evidence from the Millennium Cohort Study and Next Steps’, Journal of Prevention and Health Promotion. DOI: 10.1177/26320770231204993.
Reports
Coates, C., Patel, R. & Vanner, R. (2023) The 2023 health challenge research springboard: process and outcomes, Understanding Society Working Paper 2023-12, Colchester: University of Essex.
Johnson, E. A., Goodman, C., Swedlow, L., Hines, J., Corrigan, A., Taylor, R. & Johnson, M. T. (2023) A Big Local Basic Income: Proposal for a locally led basic income pilot, London: Compass.
Johnson, E. A., Reed, H., Nettle, D., Stark, G., Chrisp, J., Howard, N., Gregory, G., Goodman, C., Smith, M., Coates, J., Robson, I., Parra-Mujica, F., Pickett, K. E. and Johnson, M. (2023) Treating Causes Not Symptoms: Basic Income as a Public Health Measure, London: Compass.
Johnson, E. A., Webster, H. Thorold, R., Morrison, J., Mathers, A., Reed, H., Kypridemos, C., Villadsen, A., Parra-Mujica, F., Cookson, R., Nettle, D., Pickett, K. & Johnson, M. T. (2022) Challenging the Mental Health Crisis: How Universal Basic Income can address youth anxiety and depression, London: Royal Society of Arts.
Johnson, M. T., Nettle, D., Johnson, E. A., Reed, H. & Pickett, K. (2022) Winning the vote with a universal basic income: Evidence from the ‘red wall’, London: Compass.
Related links
Project website: https://www.basicincomehealth.com
Chakalian, An. (2023) ‘Is universal basic income possible here?’, The New Statesman, 08 July.
Gaumont, F. (2023) ‘Près de 1900 euros par mois, sans rien faire : le revenu universel testé en Angleterre’, Le Parisien, 17 June.
Holland, D. (2023) ‘Giving every adult £75 a week could save the NHS billions and help reduce child poverty a study has found’, Daily Express, 18 July.
Research funding and partners
2022-2023: £153,128.09 for ‘Understanding the prospective public health impact and social feasibility of Universal Basic Income schemes in the UK: Developing microsimulation of impact on self-rated health and QALYs and public engagement with “left behind” communities to understand “willingness to pay”’ from NIHR 22/38 Application Development Award (ADA): Universal Basic Income. Grant number: NIHR154451. Organisational partners: Compass and Autonomy
2022-2023: (CI) £17,000 from York Cost of Living Group (£2,000) and Newcastle University for The Changing Cost of Living study: OSF: https://osf.io/e8g3p/; Qualtrics screening survey: https://tinyurl.com/changingcostscreening; Qualtrics main survey: https://tinyurl.com/changingcost. Results tracker: https://rpubs.com/danielnettle/ccol.
2021-2022: £172,635.84 for ‘Assessing the prospective impacts of Universal Basic Income on anxiety and depression among 14-24-year-olds’, Wellcome Trust, Discretionary Award: Mental Health. Grant number: 223553/Z/21/Z. Organisational partners: RSA and Compass
